What are HPV Infections? How are They Transmitted? It Symptoms and Vaccine
Human Papilloma Virus abbreviated as “HPV” is a DNA virus. HPV infections, which develop due to the presence of this virus in the tissue, are mostly transmitted sexually and can cause genital warts and some genital cancers in women.
In this section, answers are sought for frequently asked questions such as ‘What are HPV infections, how are they transmitted, what happens once a person gets infected with HPV, how are genital warts treated, how is HPV treated’?
What is HPV?
HPV is a DNA virus that belongs to the papillomavirus family affects humans only. It has about 170 types. More than 40 of these are sexually transmitted viruses. A person can get infected with more than one HPV type at the same time. HPV infections differ from HIV and HSV infections.
What kind of complaints does it cause?
HPV infection mostly does not show any symptoms and ends spontaneously within 2 years. However, in some cases, they remain in the body and cause genital warts, genital cancer precursors and genital cancer lesions.
HPV Types
HPV -related diseases are classified into three groups as low risk, possible high risk and high risk groups.
HPV types in the Low Risk Group: Type 6, Type 11, Type 40, Type 42, Type 43, Type 44, Type 54, Type 61, Type 62, Type71, Type 72, Type74, Type 81, Type 83, Type 84, Type 91
HPV types in the Possible High-Risk Group: Type 26, Type 53, Type 66, Type 67, Type 68, Type 69, Type 70, Type 73, Type 82
HPV Types in the High Risk Group: Type 16, Type 18, Type 31, Type 33, Type 35, Type 39, Type 45, Type 51, Type 52, Type 56, Type 58, Type 59
What types of cancer does HPV cause?
HPV infections can lead to ‘oropharyngeal cancers’ involving the mouth, tonsils and throat, and ‘anogenital cancers’ involving the cervix, anus, vagina, and vestibulum region. HPV can also cause penile cancer in men.
People with low body resistance, chronic diseases, family history of cancer, and those with smoking habit are more likely to develop cancer.
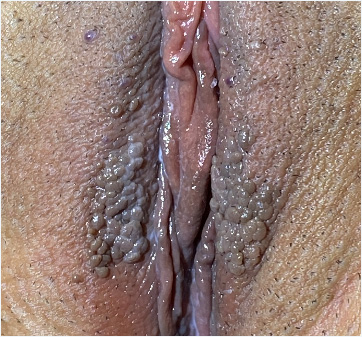
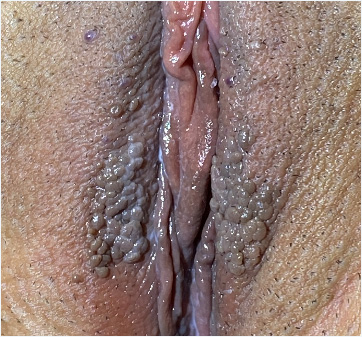
Genital wart is the name that refers to lesions in the female and male genital areas characterized by skin outgrowths caused by HPV. Genital warts may quickly spread to different areas or remain localized in a single area. They can be smaller than a grain of rice, or can reach the size of a tennis ball. Warts, which look like cauliflower with their lumpy surfaces, can be in different colors ranging from light brown to dark black. Genital warts can also spread to different parts of the body by skin-to-skin contact.
Where do genital warts develop?
Genital warts can develop in the labia minora, labia majora, clitoral hood area, perineum (between the vaginal introitus and the anus),around the anus and mons pubis. Therefore, they are also called ‘anogenital warts’. On the other hand, they can also be seen on the cervix, rectum, and inside the vagina. In men, they can also develop on and around the penis, as well. In addition, they can spread to the mouth, around the lips and even the throat, especially through oral sex.
How is HPV transmitted?
The main transmission way of HPV is sexual intercourse. Since it spreads by skin-to-skin contact, its transmission does not require sexual intercourse. It can be commonly transmitted by vaginal, anal and oral sex. HPV infection can also be transmitted from mother to baby during vaginal delivery. It rarely causes diseases in the baby. Its transmission through public toilets or objects (such as razors) is less common. It is not yet clear whether HPV can be transmitted through blood. However, some organizations in the world refuse blood donations from individuals infected with HPV.
Surgical procedures are another way of transmission of HPV infections. Health care professionals who are exposed to virus particles while treating warts are at the risk of getting infected with a kind of larynx wart called ‘laryngeal papillomatosis’.
Who are at risk?
Conditions that involve HPV risk:
- First sexual intercourse at an early age,
- Multiple sexual partners,
- Smoking addiction,
- Irregular eating habit,
- Having chronic diseases,
- Having a weak immune system.
These conditions are factors that increase the risk of transmission and the risk of disease progression. During periods of active warts, the risk of infection is at its peak. However, even in people who have HPV but do not have visible warts, it can be transmitted to the sexual partners. Since condoms do not cover the genital area completely, they can provide only partial protection, so they do not provide 100% protection against the virus.
Incidence
Sexually active women or men are exposed to this virus at least once in their life. It has been found that an estimated 291 million women in the world were infected with HPV in 2007, and that 32% of all women in the world were HPV carriers in 2011. Besides these, 9% of all men in the world are known to be HPV carriers. In fact, these consequences are inevitable because it is a sexually transmitted infection.
A study conducted in Turkey in 2019 showed that about 20% of women were HPV carriers.
What are the symptoms of HPV infection?
Even if a person gets infected with HPV, he/she may not show symptoms immediately. Its symptom onset varies depending on the condition of the immune system, age, the type of HPV, and whether there is any comorbid infection or disease. However, it should be remembered that its infectiousness continues even if there is no symptom.
How is the presence of HPV detected?
Any presence of HPV is detected by examining the swab sample taken from the cervix during the gynecological examination, with a genetic testing method called PCR. In addition, a HPV typing test can be performed on patients who tested positive for HPV (i.e. HPV +).
What happens after getting infected with HPV?
After getting infected with HPV, the virus is eliminated if the body’s immune system is adequate. If it cannot be eliminated; disease symptoms begin to appear or the virus settles in the body as a permanent infection. Such people become 'HPV carriers' and can pass the virus to their partners through sexual intercourse, even if they do not have any medical condition that causes discomfort.
HPV infections most commonly show symptoms in the form of genital warts. Patients consult a physician because of warts on their own or their partner's body. The source of this concern is the fact that even if treated, warts are likely to recur. High-risk types can cause invisible cellular changes in the cervix. Such a condition can be detected during a routine smear or HPV screening test. For further examination, the vagina and cervix can be evaluated with ‘colposcopy’.
They can also cause pain during sexual intercourse, as a result of the inflammatory process at the entrance of the vagina (vestibulum).
HPV symptoms; (Summary)
- Asymptomatic (no symptoms),
- Anogenital warts (located around the genital area and anus in women, and around the penis and anus in men).
Warts are not painful, but can cause itching problem. Genital warts may cause mild itching.
- Cervical cancers or pre-cancerous lesions,
- Warts inside the vagina or cervix,
- Pain problem during sexual intercourse due to involvement of the vestibulum (Vulvar Vestibulitis),
- Problems related to laryngeal involvement.
Protection from HPV
For protection against HPV, the followings are important:
- Use of condoms,
- Vaccination,
- Monogamous sexual relationships,
- Regular gynecological examinations and smear tests.
What is the HPV vaccine?
Vaccination is the most effective preventive method against HPV infection. The goal is the prevention of cancer and precursor lesions by providing immunization before the person’s exposure to the virus. Therefore, the vaccine should be administered before the person becomes sexually active. The effectiveness of the vaccine will be at its peak during this period.
HPV vaccines are administered to people of both genders between 9 and 26 years of age. Recent studies revealed that the vaccine could be administered to people up to 45 years of age and could remain effective.
There are 3 vaccines which provide protection against HPV infection:
- Cervarix,
- Gardasil,
- Gardasil 9.
These vaccines were approved in 2006, 2009 and 2014, respectively. Their main difference is that they are effective against different types of HPV. All of these vaccines protect against HPV types 16 and 18, which cause cervical cancer. However, Gardasil and Gardasil 9 also provide protection against HPV-6 and 11, which are the most common causes of genital warts.
How is HPV vaccine administered?
HPV vaccine is not included in the routine vaccination schedule of the Ministry of Health in Turkey. Women or men, depending on their wishes, can obtain the vaccine at their own expense, based on the doctor's recommendation.
Among the HPV vaccines, only Gardasil is currently available in Turkey. Gardasil is administered in 2 doses (first and 6th months) to those between 9-14 years of age, and in 3 doses (first, 2nd and 6th months) to those over 14 years of age. According to this protocol described as first-2nd-6th months, the second vaccine is administered 2 months after the first vaccine, and the third is administered 4 months after the second vaccine. HPV vaccines are administered intramuscularly in the deltoid region of the upper arm with a fine-tipped needle. It has been proven that the vaccine provides permanent protection and does not require repetition when administered in accordance with the specified dosage schedule.
HPV infection is today still a serious problem in some countries. The underlying causes include poor living conditions, comorbid infections such as AIDS (HIV),poor health care and difficulties in accessing the vaccine. It should be remembered that today vaccination is today the most effective preventive method against HPV infection. However, vaccination does not have a therapeutic effect after infection with HPV.
Who can be vaccinated?
Vaccination can be administered to people of both genders between 9 and 26 years of age, who have not been infected with HPV before. In recent years, it has been reported that vaccination can be administered to people up to 45 years of age. Vaccination does not have a therapeutic effect on people who have already been infected with HPV.
What should people infected with HPV do?
We recommend that they first purify themselves from the psychological effects of this disease and just have regular follow-up exams as recommended by their physicians. They can also benefit from some immune system boosting drugs and herbal products.